Known as the Pump Jack Capital of Texas, Electra is located in the north part of the state and was once a booming oil town.
“There was really no need to go to Wichita Falls for anything,” said Billy Don Clark, an Electra native and a board member of the Electra Memorial Hospital. “Anything you could think of, this town had. We had an extremely strong middle class because all of the major oil companies had offices and workers here.”
The town used to have car dealerships, a bowling alley and a drive-through movie theater. All that changed when the oil companies left in the 1970s. Today, with a population of fewer than 3,000 people, Electra has become one of many rural cities in America dramatically affected by the pandemic.
Access to quality health care has been a recurring issue for those who live in rural America, with pandemic health care providers having to find different ways to treat COVID-19 and vaccinate people in these communities.
“The pandemic changed the perception of small hospitals throughout the United States,” said Kimberly Gilbert, chief nursing officer and chief clinical officer for the Electra Hospital District. “The rural and the community hospitals were the ones that tried to take some of the pressure off of the larger hospitals and be a resource for them and keep patients in our hospital so that they could keep the sicker ones.”
Vacant buildings in downtown Electra, Texas. (Maxwell Shavers/News21)
Nonfunctioning pump jacks sit in a field in Electra, Texas. Electra was named the Pump Jack Capital of Texas in 2001, but it has since seen a decrease in population due to the waning oil industry. (Maxwell Shavers/News 21)
Even before the first COVID-19 admission at the hospital, Dr. Thomas DeLizio, chief of staff at Electra Memorial Hospital, had mapped out a plan for the pandemic.
He and his colleagues saw cases surging across the globe, overwhelming hospitals and medical workers. He knew COVID-19 would arrive in Electra soon.
“We started doing the screening where you’d make sure that the patient wasn’t having any symptoms of COVID before you let them in the building, because we didn’t want to spread COVID in our building,” DeLizio said.
The hospital also set up drive-through COVID-19 testing outside the emergency room and at a local church.
DeLizio said getting the results of COVID-19 tests was challenging at first. At the time, patient samples were sent to the Centers for Disease Control and Prevention for testing, and it would be close to a week before the results came back.

Even before the first COVID-19 admission at the hospital, Dr. Thomas DeLizio, chief of staff at Electra Memorial Hospital, had mapped out a plan for the pandemic. (Maxwell Shavers/News21)
Finding masks and ventilators also was difficult. Hospital staff had to build additional negative pressure rooms to house COVID-19 patients. Throughout the pandemic, the hospital didn’t have enough beds and had to transfer critically ill patients to a larger hospital for treatment.
The Electra Hospital District consists of three health clinics and Electra Memorial Hospital. Two of those clinics are located in Iowa Park, Texas, about a 20-minute drive from Electra.
On March 24, 2020, nurse Justin Gellner was the first staff member in the Electra Hospital District to test positive for COVID-19.
“We kept checking on my vitals to make sure everything was going to be OK. Coughing up a little bit of blood — it was a little concerning,” said Gellner, a nurse at the Park clinic. “I honestly couldn’t walk 20 foot without getting short of breath.”
On April 15, 2020, the Park clinic closed its in-patient services and transitioned to telemedicine after 75% of its staff tested positive for COVID-19.
More than a quarter of the staff employed by the Electra Hospital District has, at some point in the pandemic, been diagnosed with COVID-19, making staffing an ongoing issue.
“I had no days off, and I was probably there 7:30 (a.m.) to sometimes 7:30 (p.m.), 8 (p.m.), 9 (p.m.) at night,” said Jessi Berrett, a nurse at Electra Memorial. “Whether it was just rounding on the patients, you know, the family phone calls, actually trying to find another hospital to take a patient, procedures with patients, it was just all-encompassing.”

Nurse Jessi Berrett speaks at a COVID-19 roundtable in Iowa Park, Texas. Berrett was on the front lines of patient treatment. (Maxwell Shavers/News21)
John Perez, director of emergency medical services, said, because of staffing shortages, everyone had to pick up extra hours and work longer shifts.
Worried about putting his pregnant wife and children at risk, Perez said he got undressed in his front yard, went inside his home, threw his clothes in the washing machine and then disinfected everything he had on him: watch, keys, hat, rings.
He also bought a used RV and parked it in his backyard in case he contracted the virus and needed to quarantine.
“It was the fear of the unknown. I mean, we really didn’t have a big grasp on it. And that really was my biggest fear,” Perez said. “What I’m doing, is it enough? And then if it’s not enough, you know the what-ifs, they go forever … Really would keep you up at night. It was scary.”
Berrett said it was hard for her to see how COVID-19 affected her children at home.
“My youngest, who’s 11 now, climbed in my lap, and he’s like, ‘Mom, just stop. Don’t go back to work. I don’t want you to die,’” Berrett said.
At her daughter’s softball practices, Berrett said, other parents shunned her, accusing her of exaggerating the seriousness of COVID-19.
“Going home or to an outside environment where, like, friends and family don’t believe in it, that was infuriating,” said Laurie Portman, rehab director at the hospital. “They just didn’t see the impact that we could see.”
Before the pandemic, Berrett worked in the emergency room a couple of days a week, and she took care of most of the in-patients. One day a week she was stationed in the walk-in clinic. But when the hospital received its first wave of patients, Berrett handled all COVID-19 admissions.
Berrett and nurses called hospitals in Texas and bordering states nearly every day, searching for an open bed.
“I can tell you, we’ve spent endless hours on the phone with someone crashing next door, just begging for a bed and still being told no,” Berrett said.
Berrett said it was the first time in her career she had to discharge the healthiest patient on the floor just to make room for a sicker patient.
“That’s something that no one ever prepared me for in nursing school … to choose one (life) over another.”
A mobile clinic pulls into Alcorn State University to vaccinate student athletes in Fayette, Mississippi. The clinic provided Johnson & Johnson, Pfizer and Moderna vaccines for free. (Zach Van Arsdale/News21)
In some rural American communities, such as Fayette in Mississippi, where the population is sparse and widespread and medical staff is scarce, doctors and nurses took vaccines on the road, bringing medical care to the people rather than asking residents to come to facilities. These mobile medical units — sometimes in buses, sometimes in vans — are meant to reach people who lack transportation and other means.
“Some patients are in very, very rural areas. So transportation to the clinic may not be possible for them,” said Katrina Collins, acting CEO of Jefferson Comprehensive Health Center. “That’s how I came into play with the mobile units.”


Left: The mobile medical unit is equipped to provide primary medical care and dental care in Fayette, Mississippi. Right: The health center sends a converted RV carrying vaccines into a range of neighborhoods, from the local university campus to patients’ houses. (Zach Van Arsdale/News21)
In some cases, patients wouldn’t be able to get the vaccine if it weren’t for mobile units that go to underserved communities across the U.S.. There are an estimated 2,000 mobile clinics in the country.
“Mobile clinics are not widely supported,” according to a review in the International Journal for Equity in Health. “This has resulted in a missed opportunity to deploy mobile clinics during national emergencies such as the COVID-19 pandemic, as well as using these already existing and trusted programs to overcome barriers to access that are experienced by under resourced communities.”
More than 85% of residents in Jefferson County, where Fayette lies, are African American. Nearly 1 in 3 Jefferson County residents live in poverty, according to the latest U.S. Census report.
Collins said the mobile unit allowed the health center to provide COVID-19 testing, administer vaccinations and provide basic medical services. They also pick up patients in vans and bring them to the health center.
“We were one of the first in the area to offer rapid COVID testing,” Collins said. “We were the second in this area to offer COVID vaccines to our patients.”
A total of 728 people in Jefferson County have been infected since the pandemic outbreak.
In Jefferson County, more than 54.7% of the population over 12 years old is fully vaccinated, the second-highest vaccination rate in Mississippi, according to the CDC.
Electra Memorial Hospital plays a big role in this Texas city. The hospital employs entire families and was stretched to its limits in the peak of the pandemic. Mike Rodriguez was a patient who was on the brink of death. (Video produced by Maxwell Shavers/News21)
As the pandemic raged across the country, doctors at the Electra hospital placed patients on ventilators to keep them alive. Ultimately, seven patients were placed on ventilators.
“I wouldn’t be here today if it wasn’t for the care that I received, for the rules that were bent and persuasions that were made and everything else that was done,” said Michael Rodriguez, who was a COVID-19 patient at the hospital. “I owe Electra my life.”
His medical journey began at United Regional Hospital in Wichita Falls when he tested positive for COVID-19 on June 30, 2020.
A few days later, after he returned from his second hospital stay, Rodriguez told his wife, Melanie, he was having trouble breathing. He thought he was dying. Medical personnel at Electra Memorial Hospital put him on high oxygen flow and later on a ventilator.
At home, Melanie Rodriguez opened her door to someone from the state health department wearing a hazmat suit. She put papers on the porch and told her to sign them. The Rodriguez family was ordered to quarantine for 30 days.
“She told me I’m not allowed to leave the house,” Melanie Rodriguez said. “Nobody is. If we were, we would be prosecuted.”
“For days, we didn’t know what was going to happen,” she said. “Just with the constant transfer of hospitals and not knowing from day to day if he was going to make it.”

Michael and Melanie Rodriguez in their backyard in Iowa Park, Texas. Seven patients were placed on ventilators at the Electra hospital. Only Michael Rodriguez and one other patient survived the deadly coronavirus. (Maxwell Shavers/News21)
Hospital officials flew Michael Rodriguez, still on the ventilator, back to United Regional because it had the equipment and other resources to take care of him. His wife got a call that he would probably be on the ventilator for 12 hours.
He stayed on it for 16 days.
Once he got better, he was able to be transferred for good to the Electra hospital, where his wife believed he would get more personalized care. There, he hung a picture his youngest daughter drew for him — “You’re a fighter” — over the paper towel dispenser in his room.
Every day, he would wake up and look at the drawing for motivation.
Michael Rodriguez was finally able to return home Oct. 2, three months after contracting the virus.

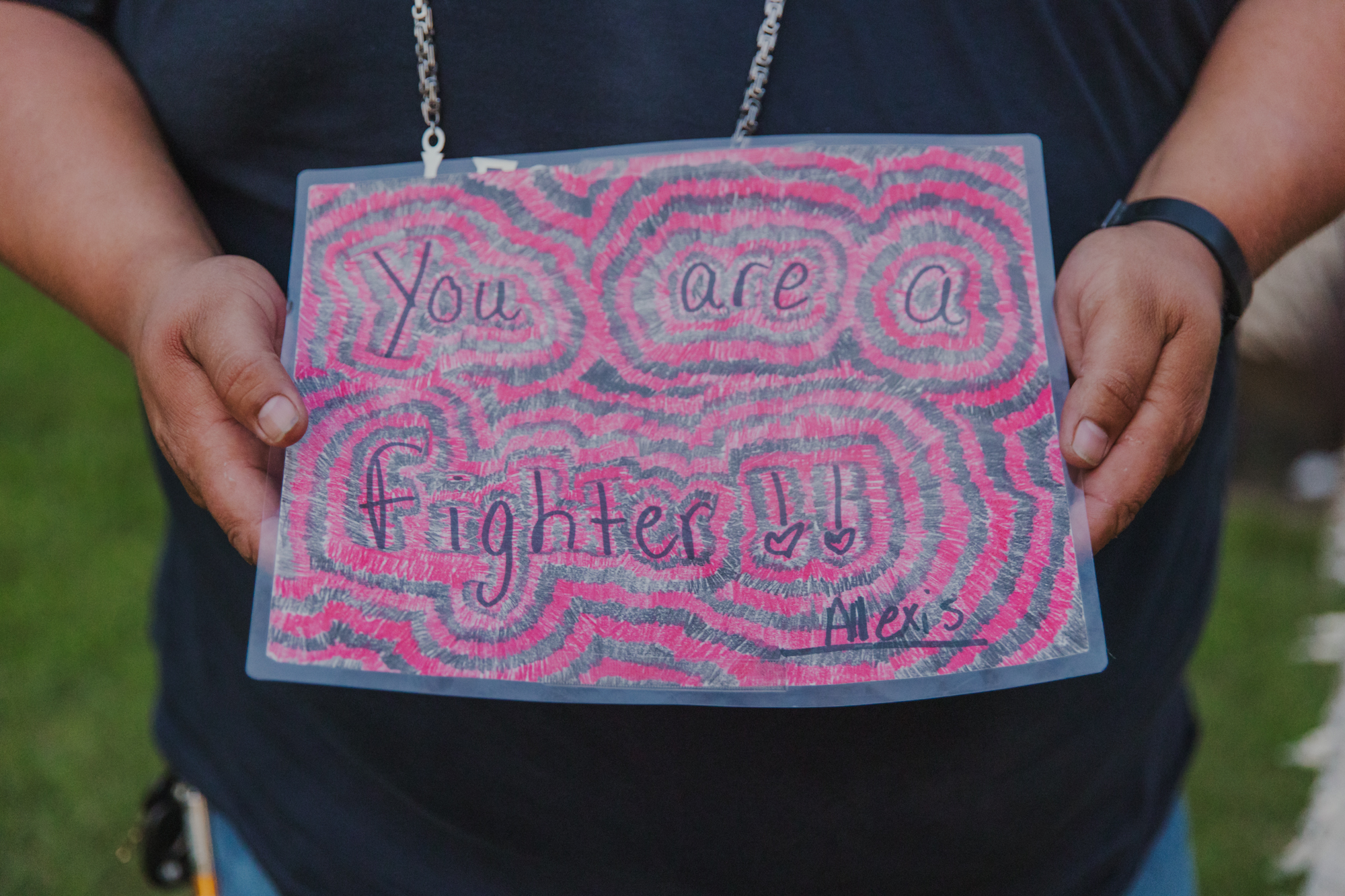
Mike Rodriguez holds a drawing made for him by his daughter Alexis in Iowa Park, Texas. Rodriguez hung the drawing on his towel dispenser while he recovered in the hospital and looked at it every morning. “It gave me the will, it gave me the fight.” (Maxwell Shavers/News21)
Nearly a year and a half of the pandemic, more than 600,000 people have died from COVID-19, according to the CDC.
Lagging vaccination rates and the highly contagious delta variant are contributing to a surge in new cases and hospitalizations, which the Institute for Health Metrics and Evaluation says could lead to an additional 76,000 COVID-19 deaths by November.
Since then, Michael and Melanie Rodriguez, and three of their children, have been vaccinated. She said their youngest will get vaccinated once she becomes eligible.
More than 165 million people in the U.S. are fully vaccinated.
The family is grateful for Michael Rodriguez’s good fortune — only he and one other person who were placed on ventilators at the Electra hospital survived.
“I did everything that they asked of me, everything they wanted me to do, pushed through everything,” he said. “I beat expectations just so that I can get home. And whenever I made it home, it was one of the most rewarding feelings that I’ve felt in a long time.”
“I fought to get out, and I still fight today.”
Michael Rodriguez still has trouble breathing. He also has nerve damage in his left leg from related complications that leaves him with little sensation below the knee.
“I’m living. I’m breathing. That’s all I need to be normal. As far as being physically back to where I was, if it happens, it happens,” he said. “As long as I continue doing what (God) wants me to do, he’ll give me what he feels I deserve.”
News21 reporters Maxwell Shavers and Zach Van Arsdale contributed to this report.